Lumbar spine pathology can affect a diverse patient population; from the young athlete, to the working adult, to the elderly patient suffering from degeneration. An initial course of non-operative treatment could include use of analgesics and NSAIDs to control pain, epidural injections, and physical methods such as bracing and flexion strengthening exercises1. However, this treatment course could be prescribed by a number of medical health care professionals. To be relevant in the Physiatry world, non-surgical treatment options need to exhibit an opportunity to improve patient function–either by reducing limiting symptoms or assisting in mobility–allowing an active return to work, sport, or daily living.
How is Physical Medicine & Rehabilitation (PM&R) Different?
Aside from a focus on non-operative treatment, one of the unique practice patterns of PM&R that helps separate Physiatry from other fields of medicine is the education and background in bracing and orthoses. In the case of lumbar spine pathology, bracing may be a key tool for improving function and reducing pain for athletes and all patients.
NASS Guidelines - Improved Function and Pain Symptoms
Referencing multiple studies, North American Spine Society (NASS) Clinical Guidelines suggest that the use of a lumbosacral corset has been shown to improve function (a significant increase in walking distance or time) and decrease pain in patients with lumbar spinal stenosis (LSS)2. In athletes, bracing has been suggested to help control pain for those with lumbar conditions including Scheuermann’s disease, scoliosis and spondylolisthesis, especially if the athlete’s symptoms have not improved with rest and activity modification3.
Furthermore, studies evaluating the influence of bracing, exercises and education found that brace treatments (done in combination with exercises) were not shown to reduce patient range-of-motion or lessen trunk strength4. In fact, non-conservative approaches are likely associated with higher risks, reported by a 2016 Cochrane Review that reiterated the high rates of side effects and complications associated with LSS surgery5.
 Setting the (Bracing) Bar Higher
Setting the (Bracing) Bar Higher
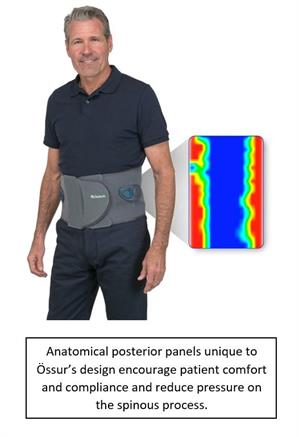
One of the newest lumbar-sacral orthoses on the market, launched by Össur on September 5th 2017, has been supported by pressure mapping data. The data demonstrated that the unique, anatomically-contoured panels of the Miami LSO™ reduce pressure on the spinous process while applying even compression on the para-spinal musculature to encourage patient comfort and compliance.
Aside from innovating clinically-indicated products, Össur’s strength is in providing business and reimbursement solutions to help practitioners develop profitable businesses. Signing up for their free Reimbursement Blog provides access to webinars, billing support, and a guide to billing for spinal orthosis under Medicare.
Lumbar Bracing and Injections
More Physiatrists are utilizing injections as an alternative to opioids and other pain medications for treatment of lumbar spine pathology symptoms. Although no randomized-controlled trials were found showing the efficacy of lumbar bracing in combination with injection treatments, similar protocols exist for other joints including the hip, knee and ankle. With positive clinical and anecdotal data for both treatments, the combination of injections and lumbar bracing could provide a solid platform for conservative rehabilitation of the pathological lumbar spine patient.
To learn more or request a product demonstration, visit www.ossur.com/miami-lso
References:
- Kalichman L & Hunter, DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. European Spine Journal. 2008;17(3): 327–333
- North American Spine Society. Evidence-based Clinical Guidelines for Multidisciplinary Spine care: Diagnosis and Treatment of Degenerative Lumbar Spinal Stenosis. 2011: 51-54. Retrieved from https://www.spine.org/Documents/ResearchClinicalCare/Guidelines/LumbarStenosis.pdf
- Baker, RJ & Patel, D. Lower Back Pain in the Athlete: Common Conditions and Treatment. Prim Care Clinical Office Practice. 2005;32: 201–229
- Spratt KF, Weinstein JN, Lehmann TR, Woody J, Sayre H. Efficacy of flexion and extension treatments incorporating braces for low-back pain patients with retrodisplacement, spondylolisthesis, or normal sagittal translation. Spine. 1993;18:1839–1849
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database of Systematic Reviews. 2016;1 DOI: 10.1002/14651858.CD010264.pub2.
- Data on file at Össur