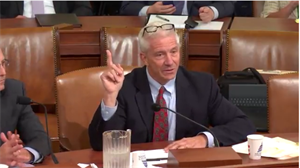
 On Wednesday, September 7, AAPM&R President, Greg Worsowicz, MD testified at the U.S. House of Representatives Ways and Means Committee's Health Subcommittee hearing on Incentivizing Quality Outcomes in Medicare Part A. His testimony placed an emphasis on improving the quality and efficiency of patient care through payment reform measures and value-based purchasing in the post-acute care (PAC) sector.
On Wednesday, September 7, AAPM&R President, Greg Worsowicz, MD testified at the U.S. House of Representatives Ways and Means Committee's Health Subcommittee hearing on Incentivizing Quality Outcomes in Medicare Part A. His testimony placed an emphasis on improving the quality and efficiency of patient care through payment reform measures and value-based purchasing in the post-acute care (PAC) sector.
Read his full statement and watch the hearing.
Learn more about how AAPM&R is working to advance and protect the specialty.
Below is the statement released by the Ways and Means Health Subcommittee:
Today, the Ways and Means Health Subcommittee, chaired by Rep. Pat Tiberi (R-OH), held a hearing to examine whether existing Medicare Part A policies are improving the quality and cost-efficiency of care in hospitals. Specifically, Members heard from physicians, researchers, and administrators about opportunities to improve post-acute care settings—such as home health agencies, long-term care hospitals, or skilled nursing facilities—to deliver better outcomes for patients.
As Chairman Tiberi said at the start of the hearing:
“We are all here for the same reason today: to explore ways to better improve the quality of care for Medicare patients.”
Building off of Congress’ successful effort to modernize the way Medicare pays physicians, Ways and Means Committee Chairman Kevin Brady (R-TX) added:
“Today’s hearing is a valuable opportunity to examine how existing Medicare policies are incentivizing hospitals and post-hospitalization providers to deliver high-quality, cost-efficient care …
“Physician payment policies are just one piece of the puzzle. To ensure the Medicare program is truly delivering the high-quality care seniors deserve, we also need to improve the way it pays post-acute, or after hospitalization providers.”
As the Ways and Means Committee takes steps to improve the Medicare Part A program, Members on both sides of the aisle asked witnesses what recommendations they have for incentivizing higher-quality care in post-acute settings so patients receive the treatment they need at a cost they can afford.
As Steve Guenthner, president of a post-acute care provider known as Almost Family, said:
“Value-based purchasing is the natural next step in the evolution of patient-centric Medicare policy, especially when it rewards providers for patient-focused outcomes, balanced against the cost incurred to achieve those outcomes … We need to change the policy question from ‘how should we pay providers’ to ‘how we should care for patients.’”
Looking at past reforms to incentivize quality in Medicare, such as with the IMPACT Act, Dr. Barbara Gage from George Washington University, explained:
“Tying [Medicare] payments to minimum quality thresholds to ensure that services are appropriate and cost effective is key to effectively redesigning the Medicare program in a way that ensures beneficiaries have access to the appropriate services they need.”
Elisabeth Wynn, who oversees health economics and finance at the Greater New York Hospital Association, added:
“We strongly encourage you to adopt reforms that consolidate the hospital [pay-for-performance] programs similar to the approach adopted for physicians to streamline the programs, balance the incentives, and improve the fairness.”
Dr. Gregory Worsowicz, who is chairman of the board for the American Academy of Physical Medicine and Rehabilitation, agreed:
“I would ask you, whatever programs we put in place, we coordinate them … we don’t suboptimize what we are doing and restrict [doctors] with so many regulatory issues [they’re] hamstrung on what [they] can do or chasing incentives that may not align with others.”
These are the types of important reforms Chairman Brady and Rep. Ron Kind (D-WI) are working to advance through their bill, the Medicare Post-Acute Care Value-Based Purchasing Act of 2015. As the Chairman explained:
“By providing the right incentives, this legislation will bring increased competition and innovation to Medicare while lowering costs to the program. At the same time, the bill will raise the bar for patient care nationwide. It rewards providers who set themselves apart in delivering excellent care to Medicare patients.”
In the weeks ahead, Ways and Means Members will explore ideas, such as those introduced by Chairman Brady and Rep. Kind, to reward quality, innovation, and excellence in health care within post-acute care services.