The Activity Tracker Explosion and What This Means for the Rehab Patient Population
 Allison Nuovo, MD
Allison Nuovo, MD
PGY2, University of Utah
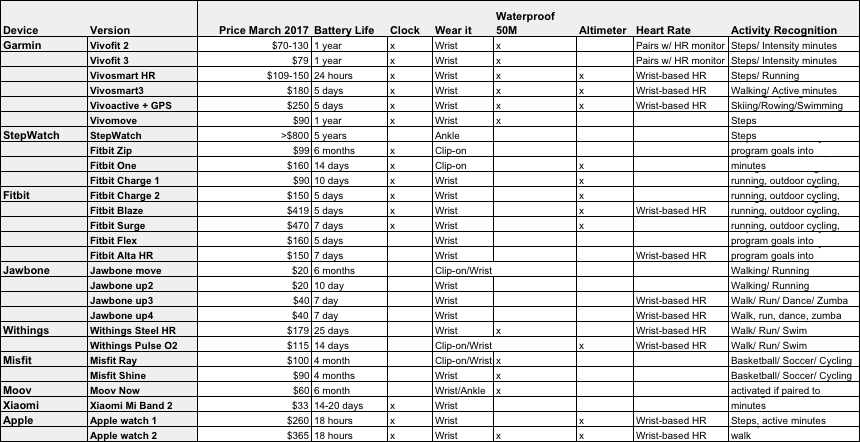
Tracking personal fitness is all the rage. For this article, I made an effort to compile all the current electronic activity monitors (EAMs) on the market in a spreadsheet, and found the task impossible! Forbes estimates this trend to continue, anticipating 411 million smartwatches will be sold in the year 2020. While almost all EAMs contain a 3-axis accelerometer to measure steps per day, many have additional gadgets like altimeters to track floors climbed and elevation gained, infrared light sensors to assess heart rate without a chest strap, algorithms to estimate energy expenditure and sleep, and one brand even includes a built-in pulse oximeter.
Increasing physical activity in rehab patients is a great goal considering sedentary behavior dominates despite our efforts to increase physical activity on the acute inpatient rehab unit. A study published in 2015 suggests stroke patients on acute rehab may spend as much as 93% of their hospital stay either sitting or lying down7. Physical inactivity is a modifiable risk factor for several medical conditions including stroke6. EAMs may help motivate our patients to get active. However, wearing an accelerometer alone may not do anything as highlighted by the 2008 study, “How active are people with stroke? Use of accelerometers to assess physical activity.”
The psychology of behavior change suggests people need a component of self-monitoring (provided by tracking daily steps on a device, for example) and additionally require ongoing feedback, social support, structure, specific goals, and goals review3. As physiatrists, we may use these EAMs to check in on our patients remotely and provide feedback or assess their physical activity progress. We can use these to monitor prosthetic use in amputees, to see if their prosthetic is helping a patient ambulate more or if it is not fitting well, they might ambulate less. Certain commercial trackers are geared toward looking at intensity minutes and have built in alternate activities like cycling, swimming etc., which would work better for those who are largely not ambulatory like the spinal cord population. We may also use these to evaluate progression of neurologic diseases such as Parkinson’s, MS, and muscular dystrophies, because over time it will be more challenging for these patients to ambulate as they once did2.
There are a few published systematic reviews that look at the reliability and validity of these commercial devices, though they are generally toward more popular tracker giants like Fitbit, Apple Watch, and Jawbone1,6. While these commercial trackers are not as accurate at tracking steps as research-grade devices like the StepWatch and Actigraph, they are a fraction of the cost and have user-friendly smartphone applications. If used for overall physical activity monitoring, these commercially-available products perform well, though the add-on features like calorie counting may provide questionable data.
However, one potential problem for our patients who want to use these devices is their variability in gait and gait speed. All accelerometers have a threshold to detect activity and if this threshold is too high, it may not detect a slower individual’s activity. I have seen a study that suggests commercial accelerometers still have the capacity to work for patients with varied gait and speed, but these studies generally examined high-functioning patients with a gait speed of approx. 2 mph1. More studies are needed to examine the use of commercial EAMs in people with varied gait, gait speed, and even no-gait in wheelchair mobility. Despite this, EAMs may be a useful tool for the rehab population going forward.
A Comparison Chart for Current Popular Electronic Activity Trackers
For those interested in researching this topic further:
- Accuracy of 2 Activity Monitors in Detecting Steps in People With Stroke and Traumatic Brain Injury. Fulk G, Stephanie A. Combs K. Physical Therapy Feb 2014
- Advances in wearable technology and applications in physical medicine and rehabilitation: The potential impact of wearable technology on physical medicine and rehabilitation. Bonato P. In Journal of NeuroEngineering and Rehabilitation (2005)
- Behavior Change techniques implemented in electronic lifestyle activity monitors: a systematic content analysis. Lyons E, Lewis Z, Mayrsohm B, Rowland J. Journal of Medical Internet Research (2014)
- How active are people with stroke? Rand D, Eng JJ, Tang PF et al. Stroke, Dec 2009; 40:163-168
- Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Feigin VL, Forouzanfar MH, Krisnhamurthi R, Mensah GA, Connor M, Bennett DA. Lancet 2014;383:245-55.
- Systematic review of the validity and reliability of consumer-wearable activity trackers. Evenson K, Goto M, Furberg R. International Journal of Behavioral Nutrition and Physical Activity. Dec 2015; 12:159
- Use of accelerometers to examine sedentary time on an acute stroke unit. Mattlage A, Redlin S, Rippee M et al. J Neurol Phys Ther. 2015 Jul;39(3):166-71.
- Validity of Different Activity Monitors to Count Steps in an Inpatient Rehabilitation Setting. Treacy D, Hassett L, Schurr K, et. al. in Physical Therapy (2017)