In early September, the Centers for Medicare and Medicaid Services (CMS) released 2024 Merit-Based Incentive Payment System (MIPS) performance feedback and final scores to MIPS eligible clinicians. These scores will impact 2026 Medicare Part B payments. Around the same time, the American Medical Association (AMA) identified several issues with MIPS cost measures, which might be contributing to unfair scores and penalties. The AMA also found that these issues are not limited to a single cost measure or specialty, and that they are difficult to assess fully due to incomplete information in the feedback and accompanying reports.
To help with their advocacy efforts, the AMA is seeking the help of other specialty societies to pinpoint where MIPS cost measures and feedback reports may be falling short. They are specifically interested in learning more about:
- Whether physicians are being penalized for costs or services that are beyond their control.
- Whether appropriate adjustments are being made for differences in patients that inherently require more services or more expensive services.
- How often physicians are being held accountable for the costs of patients attributed to them solely because of a single exam or consultation.
If you participated in MIPS in 2024 and are willing to contribute to this effort, AAPM&R is requesting that you download and send de-identified versions of your 2024 MIPS performance feedback reports to share with the AMA.
What Data Would You Like Me to Share?
- De-identified PY 2024 Final Performance Feedback Report
- De-identified Episode-Level Reports
- De-identified Supplemental Cost Reports
How Do I Access MIPS Feedback Reports?
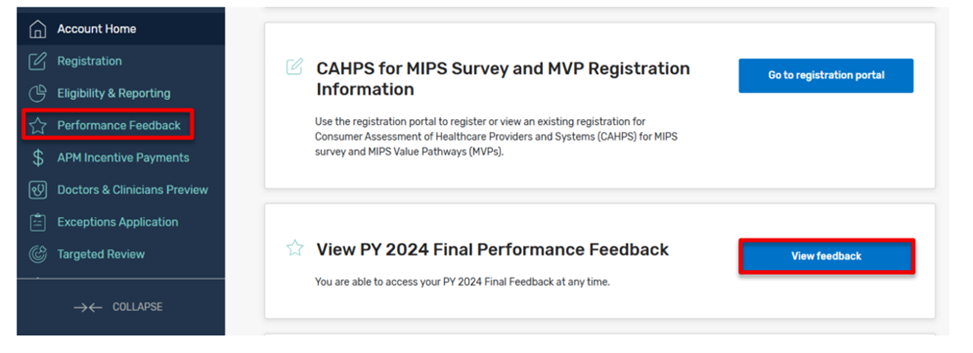
- Sign in to
the Quality Payment Program (QPP) website using your Health Care
Quality Information Systems (HCQIS) Access Roles and Profile (HARP)
system credentials; these are the same credentials that allowed
you to submit your 2024 MIPS data. A user guide with instructions
on how to access this system is available for download here.
- Once
logged into the secure QPP website, click “View Feedback” on the
home page and select your organization (Practice,
Alternative Payment Model (APM) Entity, Virtual Group).
- Practice representatives can access individual, subgroup, and group feedback.
- Third party representatives can’t access final feedback or payment adjustment information
Once you have clicked on “view feedback” and select an affiliated
practice, you should be able to view your 2024 final scores in each of
the four MIPS performance categories, as well scores on each measure and
activity you or your group reported or were evaluated on. Please download this full report and de-identify/black out any information you do not wish to share.
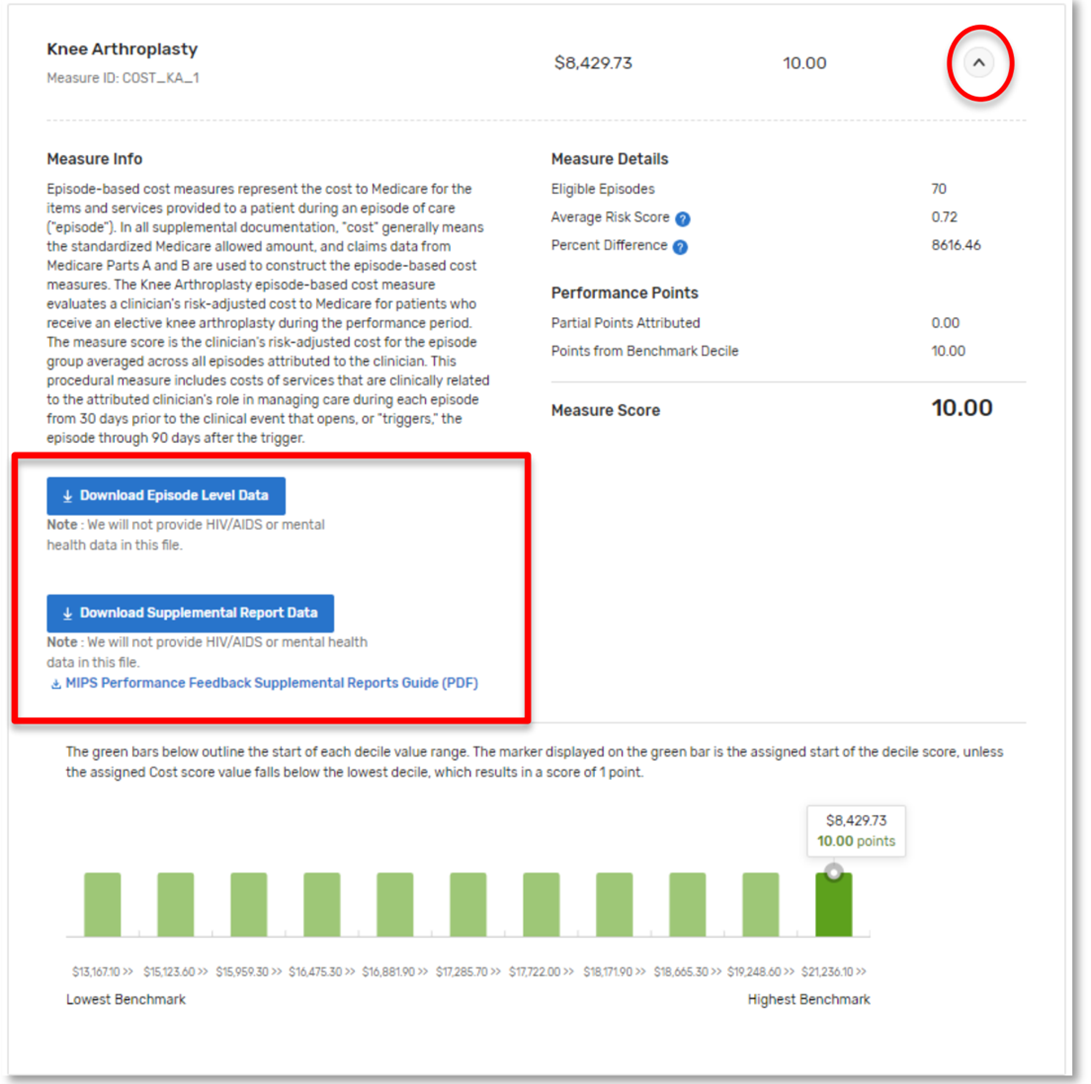
Clinicians
and groups who were scored on at least one cost measure should also be
able to access more specific cost measure information in their
performance feedback report, as shown below. Please
download your practice’s episode level data and supplemental report data
by clicking on the links highlighted below, and de-identify/black out
any information you do not wish to share.
Where Can I Find Additional Information?
CMS offers numerous guidance documents through its QPP Resource Library to help you access and interpret your MIPS feedback reports:
Please send these reports to AAPM&R no later than Thursday, December 4, 2025. Reports and any questions should be sent to healthpolicy@aapmr.org.