Stroke remains the second leading cause of death, the third leading cause of death and disability combined1, and a leading cause of institutionalization in the world. Developed by the Academy’s Innovative Payment and Practice Models (IPPM) Committee, the Stroke Rehabilitation Toolkit is a clinical and educational resource that AAPM&R members, payers, and health care systems can utilize to develop care structures and alternative payment models (APMs) to allow for the provision of high value stroke rehabilitation care.
This toolkit offers members the tools they need to develop a physiatrist-led stroke rehabilitation APM, in which clinical outcomes and patient satisfaction will improve and costs will be reduced through consistent and direct involvement of physiatry in stroke rehabilitation care across the continuum.
Highlights from the AAPM&R Stroke Rehabilitation Toolkit include:
Description of the Economic Considerations
To effectively improve stroke rehabilitation value, one must consider not only clinical factors but also the economic model in which one is practicing.
- Understand the current models of care and its financial arrangements for alternative payment structures, which include accountable care organizations (ACOs), bundled payments, shared savings arrangements, integrated delivery and finance systems (IDFS) and “one-sided” and “two-sided” risk.
Innovative Care Pathways
To effectively improve stroke rehabilitation value, one must understand that evolving from a fragmented to a seamless model of care requires innovation.
- Ensure that a seamless continuum of stroke rehabilitation care requires development of a biopsychosocial model that incorporates clinical guidelines and performance indicators that are biomedically oriented and takes into account language and educational barriers and economic and cultural differences. Standardized decision trees using evidence-based medicine for level of care transitions, stroke rehabilitation protocols, and interdisciplinary approaches of care helmed by physiatrists need to be established.
Innovation of a stroke rehabilitation continuum of care needs to extend beyond the walls of IRFs, skilled nursing facilities, home health services, and outpatient therapy services, into areas of telehealth and other digital platforms.
Current Environmental Assessment
To effectively improve stroke rehabilitation value, one must assess the existing healthcare environment before, while, and after building a stroke rehabilitation APM.
- Learn the framework to conduct an internal assessment of strengths and challenges and regional assessment of opportunities and threats to assist one’s program in determining their most appropriate next strategic steps.
This approach enables the model to gather a broad range of information about its current functioning, and allows leadership to consider strategies to mitigate risk, improve market share and address deficits.
Essential Components of an Effective Organizational Team
To effectively improve stroke rehabilitation value, one must build an effective organizational team comprised of both clinical and non-clinical stakeholders.
- Consider the elements of building a team of critical stakeholders, engaging providers in change, and providing support to achieve the mission of the APM.
Engaging Senior Leadership in APM Adoption
To effectively improve stroke rehabilitation value, one must prioritize the direct engagement of senior leadership.
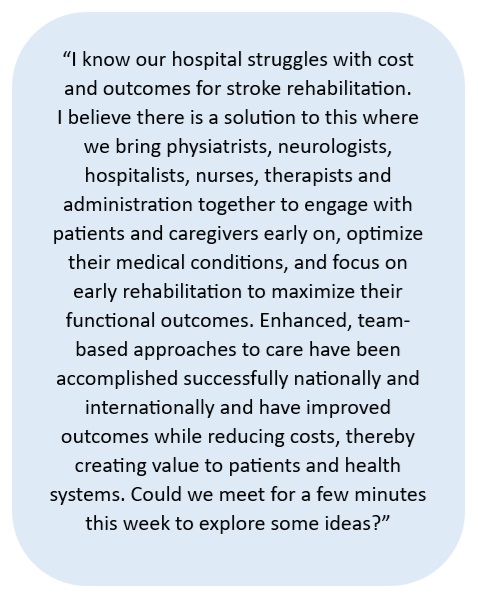
- Understand the steps in obtaining buy-in and involvement of senior leadership through studying the institution or system’s mission and core values and creating an elevator pitch to justify the need for an APM.
Recommendations for Quality, Clinical, and Financial Outcome Metrics, Data Analysis, and Program Assessment
To effectively improve stroke rehabilitation value, one must consider outcomes data that is relevant to both the patient and the model.
- Identify the different types of outcome measures (structure, process, and outcomes), structures of data (registries), and examples of measures (PROMIS, ODI, Roland Morris Disability Questionnaire, Visual Analog Score for pain, Short Form 36 Health Survey, and Euro-QOL 5D).
Identify Key Clinical Team Members and Their Roles
To effectively improve stroke rehabilitation value, one must create a list of clinical team members whose input is essential to establish and run a stroke rehabilitation APM.
This may include:
|
✔ Physiatrist
✔ Occupational Therapy
✔ Social Work, Case Managers
|
✔ Rehabilitation Nurses
✔ Speech Language Pathology
✔ Psychology, Neuropshychology
|
✔ Physical Therapy
✔ Nutritionist/Dietician
✔ Vocational Rehabilitation
✔ Other Physician Specialties
|
Considerations in Care Pathway Development
To effectively improve stroke rehabilitation value, one must consider care pathways as a way to ideally integrate evidence-based medicine and utilize exemplary or best practices to manage patient care, diminish variation, advance quality, and increase efficient use of healthcare resources.
- Distinguish the components of a seamless stroke rehabilitation continuum of care, including criteria for entry to, care transition in, and exit from the APM.
Recommendations for Increasing Awareness and Influence of Program
To effectively improve stroke rehabilitation value, one must consider opportunities to increase awareness.
- Learn how to engage and increase awareness of APM at local, regional, and national levels.
1GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795–820.