Menu
Merit-Based Incentive Payment System (MIPS)
The framework for the Quality Payment Program (QPP) was established under the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 as an effort to shift Medicare physician payment towards value-based care. A core component of the QPP is the Merit-Based Incentive Payment System (MIPS), which is a performance-based payment adjustment system for Medicare Part B providers.
MIPS Performance Categories
Under MIPS, clinicians are evaluated and receive an adjustment to their Medicare Part B payments based on their overall performance across four performance categories:
1: Quality: Evaluates performance on a set of quality measures, which can include outcome, patient experience, and care process measures.
2: Improvement Activities: Addresses efforts to enhance clinical practice and support patient engagement.
3: Promoting Interoperability: Focuses on electronic exchange of health information using certified electronic health record technology (CEHRT) and promotion of patient engagement.
4: Cost: Assesses cost of care provided for certain episodes of care (based on Medicare claims).
Based on performance across these four categories, clinicians can receive either a positive, neutral, or negative adjustment to their Medicare Physician Fee Schedule payments. Eligible clinicians who do not comply with the program are subject to a -9% payment adjustment.
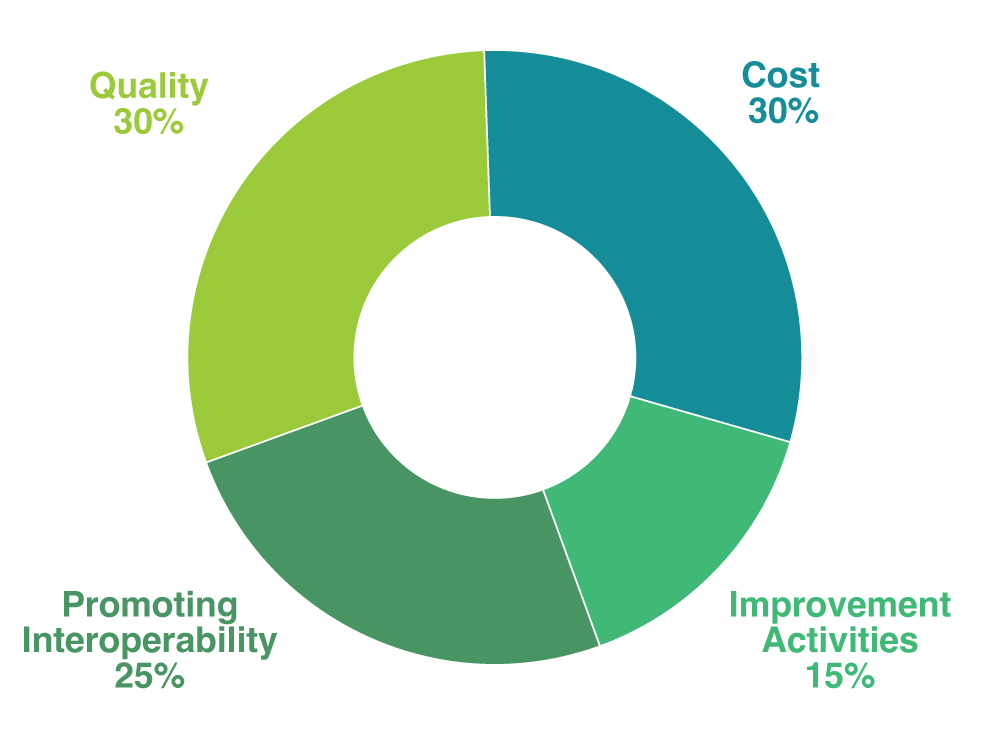
Note that in specific circumstances, these weights could vary. For example, MIPS eligible clinicians who meet CMS’ definition of small practice, hospital-based, or ambulatory surgical center-based are automatically exempt from the Promoting Interoperability category, in which case, the category’s 25% weight is redistributed to another performance category (or categories). For more information on CMS’ MIPS performance category redistribution policies, click here.
MIPS Eligibility
MIPS reporting is required for most Medicare Part B providers with some exceptions.
There are three exclusions from MIPS eligibility, which may be applied at the individual clinician or the group level:
- Advanced Alternative Payment Models (APMs): Providers who have achieved sufficient participation in an Advanced APM, as defined by MACRA, are not subject to MIPS.
- Low Volume Threshold: Providers who meet at least one of the following criteria can be excluded from MIPS.
CMS will conduct low-volume status determinations prior to and during the performance period using claims data. If a provider exceeds one or two of the above criteria, but not all three, they are not required to participate in MIPS but may choose to “opt-in.”
- New Medicare-enrolled Eligible Clinicians: Providers who enroll in Medicare for the first time during a performance year are exempt from MIPS until the next subsequent performance year.
Look up if you need to participate in MIPS
MIPS Participation Options
MIPS eligible clinicians have five options for participation:
- Individual: A clinician that submits individual performance data.
- Group: A practice that submits aggregated performance data on behalf of all clinicians billing under its Tax Identification Number (TIN).
- Virtual Group: A combination of two or more TINs that elect to form a virtual group.
- Subgroup: A subset of clinicians in a group (only applicable to those participating through a MIPS Value Pathway).
- APM Entity Group: A clinician or group of clinicians who are participating in an APM.
Requirements will vary based on the participation options, as discussed in the Performance Category resources linked above.
MIPS Reporting Options
MIP eligible clinicians have three options for reporting:
- Traditional MIPS: Clinicians select the quality measures and improvement activities that they will report on for the performance year. Clinicians also report the complete Promoting Interoperability measure set. CMS collects and calculates the cost performance category.
- MIPS Value Pathways (MVPs): Starting in 2023, MIPS eligible clinicians, group practices, subgroups of TINs, and APM Entities have the option to participate in MIPS under a new framework known as MIPS Value Pathways or MVPs. MVPs are intended to streamline the MIPS participation experience by connecting activities and measures across the four MIPS performance categories that are relevant to a specific specialty, condition, or population. Learn More About MIPS Value Pathways!
- APM Performance Pathway (APP): The APP is a streamlined reporting option for clinicians participating in a MIPS APM. Under the APP, participants report a predetermined, primary care-focused measure set in addition to the complete Promoting Interoperability measure set (reported under Traditional MIPS).